Starting the New Year off with a happy topic…
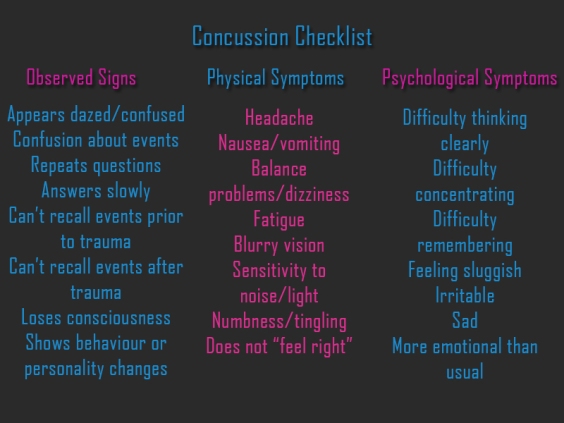
A concussion is considered to be a minor traumatic brain injury. For the 48 hours following a concussion/blow to the head, careful monitoring should be carried out because there is an overlap between symptoms of concussions and haematomas/haemorrhages (bleeds on the brain). However, if a brain scan is carried out and there’s no bleeding or swelling only then can concussion be diagnosed. Generally a concussion isn’t a huge source of worry, but evidence has suggested repeated concussions can cause long term problems with mental abilities and trigger a form of dementia called chronic traumatic encephalopathy. This is a particular issue in athletes who suffer repeated severe concussions.
Delving a little further into the causes of concussion , it occurs when a sudden impact causes a disruption to the reticular activating system (RAS) in the center of the brain. This area helps to regulate awareness and consciousness; for example sleep cycles, attending to important information such as your name being called in a busy doctor’s surgery. If a head injury is severe enough to cause a concussion, the disruption in the brain cells triggers symptoms such as loss of memory and mental confusion.
, it occurs when a sudden impact causes a disruption to the reticular activating system (RAS) in the center of the brain. This area helps to regulate awareness and consciousness; for example sleep cycles, attending to important information such as your name being called in a busy doctor’s surgery. If a head injury is severe enough to cause a concussion, the disruption in the brain cells triggers symptoms such as loss of memory and mental confusion.
Certain sports have a higher-than-average risk, including rugby, boxing, cycling, and martial arts. It’s argued that the benefits of regularly engaging in these sports outweigh potential concussion risks, particularly if correct equipment is worn. However, boxing is highlighted by doctors as dangerous because the risks of serious brain injury are unacceptably high – the aim of the game is to beat the crap out of each other after all. (We’ll get to concussions in hockey in a later post and why it’s a hot topic currently!).
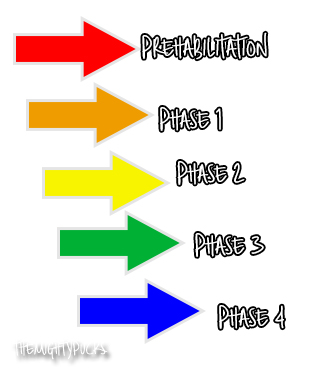
Mild concussions can be treated with self-care techniques such as a cold compress to reduce swelling, paracetamol for pain relief, rest, avoiding alcohol and drugs, and no contact sports. There is no definitive agreement on when one can safely return to sports following a concussion. The general steps are to wait until symptoms have passed for at least 24 hours then light exercise can be brought in, sport specific exercises (that exclude any impact to the head), non-contact training then full training with a return to play. However if symptoms re-emerge then take a step back. A concussion takes – on average – 7 to 10 days to recover fully.
It is worrying though that despite the awareness and research that has gone into concussions, we still do not have anything particularly concrete on them. Are certain individuals susceptible? Could we develop a biomarker to definitively diagnose a concussion? What about a treatment that actually does something rather than rest and gradual return?
Post-concussion syndrome (PCS) is used to describe symptoms that last for several weeks or months but the exact cause is poorly understood: There are thoughts that it could be a result of damage to nerve cells in the brain or a chemical imbalance triggered by the initial injury. The majority of PCS cases resolve within three to six months, and treatments for specific symptoms can be used to alleviate it, for example migraine medication for headaches or anti-depressants for depression. [X]